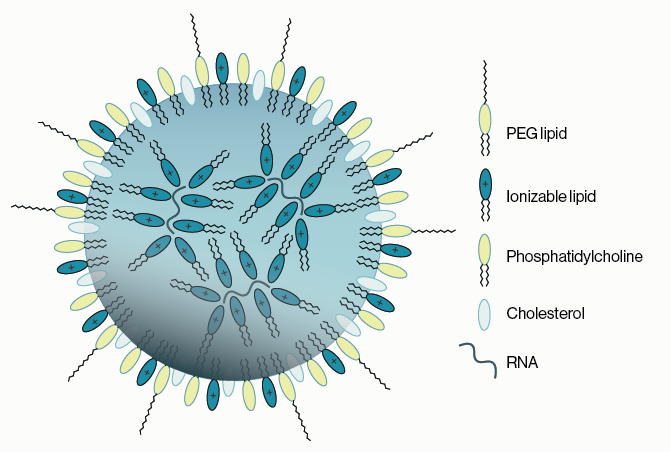
Alcohol consumption is an ongoing public health issue that represents up to five percent of the global disease burden. Clinical evaluation of alcohol abuse has historically relied upon measurement of serum liver enzymes of corpuscular volume of red blood cells. However, these measures can often be inaccurate owing to other health complications that often overlap with heavy alcohol use. More recent analyses have begun to make use of alcohol metabolites as biomarkers for alcohol use. One of these is a phospholipid named phosphatidylethanol, aka PEth, which is produced from phosphatidylcholine via phospholipase-d (PLD). Under normal conditions in the presence of water, PLD converts phosphatidylcholine to phosphatidic acid. However, PLD can also utilize ethanol which generates a different modification to the lipid headgroup and results in PEth (Figure 1).
Evidence suggests that the accumulation of PEth in the membranes of neural cells leads to competition with endogenous agonists of ion channels. This is thought to significantly contribute to intoxication from alcohol consumption. While cellular build-up of PEth levels is obviously undesirable, its propensity to be integrated into cellular membranes actually lends to its use as a biomarker.
Figure 1: Schematic of the action of PLD on phosphatidylcholine. Phosphatic acid and phosphatidylethanol are alternately produced depending on the use of water or ethanol, respectively, in the reaction.
Utility as a Biomarker
The stable incorporation of PEth into membranes contributes to its clinical utility in two ways: 1) it can be found readily in red blood cells (RBCs) and 2) its half-life is approximately 10 days. Other alcohol metabolites such as ethyl glucuronide (EtG) are comparatively short-lived, with a half-life of less than one day. The stability of PEth in the blood allows for a long 'look back', i.e. a greater window for detecting prior episodes of increased alcohol use. Testing for EtG is also problematic due to sensitivity to other sources of ethanol.
As mentioned above, serum proteins such as carbohydrate deficient transferrin can be used as an indirect biomarkers of alcohol use. However, these have a low correlation to total ethanol consumption and are prone to false positive results due to other common health issues. Conversely, PEth is a direct biomarker for alcohol use and circulating PEth levels have been shown to be directly correlated to blood alcohol levels.
The long half-life of PEth and its high degree of association past alcohol use arguably make it the ideal biomarker for clinical evalutaions.
Methods of Analysis
There are several obstacles to PEth analysis. First and foremost, is dealing with efficient extraction of the sample. RBCs are known to have a complex cellular matrix that can often occlude downstream analysis of certain analytes so care must be taken to optimize extraction of the sample. One of the current prevailing methods for preparing RBCs is applying whole blood to dried blood spot (DBS) cards. Dried blood can then be efficiently extracted, often in a single step, with organic solvents that contain an internal standard for the target analyte.
This extraction method has been successfully paired with modern mass spectrometry (MS) methods for PEth analysis. Key to this has been the advance of sensitivity within MS methods. As liquid chromotography coupled MS has pushed forward to ultra high performance liquid chromatography (UHPLC) paired with tandem mass spectrometry (MS/MS), so has the limit on PEth detection been pushed down. Current sensitivity limits are under 10 ng/mL. This enables sensitive, quantitative discrimination of non-drinkers (<8 ng/mL) from even low-level consistent drinkers (20-50 ng/mL).
Outside of MS, detection of PEth has been more difficult. Antibody based methods are available but currently suffer from a lack of sensitivity in clinically relevant applications. Similarly, ELISA methods for PEth detection are available, but direct comparison of samples to a standard curve remains qualitative.
Clinical Outlook
The need for clinical analysis of ethanol metabolites is unlikely to decrease soon. Furthermore, given the advantages outlined above, PEth is likely to remain the metabolite of choice for clinical analysis. MS will also continue to be the method of choice for PEth analysis. This is not only due to the sensitivity of the method but to its acceptance as a quantitative standard in forensic toxicology labs capable of performing legally adequate analyses. The primary disadvantage of MS is it remains a low-throughput method that is relatively expensive in terms of dollars per sample.
Methods for implementing primary screening of samples for alcohol use could potentially greatly reduce the number of samples that need quantitative values via MS for legal means. Hypotetically, quantitiative values for abstinence monitoring are only necessary below certain cutoffs for ng of PEth per mL of blood. This cutoff varies some, but generally falls between 20-50 ng/mL, with values consistently above this range being indicative of continued alcohol use or abuse. From this perspective, a quantitative value above this threshold may not be practically useful since a positive test at 100 ng/mL would legally be the same as a positive test at 500 ng/mL. If alternative methods that are compatible with high-throughput methods, such as the ELISA, could be improved in terms sensitivity and quatification, it would enable the ability to rapidly rule out a large majority of samples for MS spec testing and in turn reduce costs associated with alcohol use monitoring.
Learn more about our PEth ELISAReferences
1. Odoardi S et al. (2014) Simplifying sample pretreatment: Application of dried blood spot (DBS) method to blood samples, including postmortem, for UHPLC–MS/MS analysis of drugs of abuse Forensic Science International 243; 61-67
2. Zakaria et al. (2016) Advantages and Challenges of Dried Blood Spot Analysis by Mass Spectrometry Across the Total Testing Process EJIFCC. 2016 Dec; 27(4): 288–317.
3. Neilsen et al. (2019) Alcohol + PLD = Phosphatidylethanol, a Long‐Term Alcohol Biomarker Vol 33, Issue S1 Experimental Biology 2019 Meeting Abstracts; 635.16-635.16
4. Johannson et al. (2020) Phosphatidylethanol Levels, As a Marker of Alcohol Consumption, Are Associated With Risk of Intracerebral Hemorrhage Stroke 51:2148–2152.
5. Stewart et al. (2014) Validation of Blood Phosphatidylethanol as an Alcohol Consumption Biomarker in Patients with Chronic Liver Disease Alcohol Clin Exp Res. 38(6): 1706–1711
0.2
/ 0.3
Related Articles
Stay informed with our informative blog posts.
0.3
/ 0.3
Get in Touch
If you have any questions or would like to learn more about our services, feel free to reach out to us. We’re here to help!
Biosciences